Skin Cancer Treatment
Why Have a Facial Plastic Surgeon treat skin cancer?
The number one goal of removing a skin cancer is a complete excision of the lesion. There are several types of specialists (e.g. facial plastic surgeons, plastic surgeons, dermatologists) who are well qualified to remove skin cancers and achieve an acceptable cure rate. The question is, who will get the best result?
Facial plastic surgeons are uniquely qualified not only to fully excise a skin cancer but to also repair the defect in a manner that has the most aesthetically pleasing result. After completing an approved residency, usually in Otolaryngology, Head & Neck Surgery, a facial plastic surgeon completes a rigorous Facial Plastic & Reconstructive Surgery fellowship, followed by a comprehensive oral and written exam. With the knowledge of the underlying structures of the face and neck coupled with the additional training, a facial plastic surgeon is able achieve a cure with minimal disfigurement.
How is skin cancer diagnosed and treated?
Skin cancer is diagnosed by removing all or part of a growth and examining the cells under a microscope (biopsy). Skin cancer can be treated by a number of methods, depending on the type of cancer, its stage of growth, and its location on the body. Dr. Lieberman and Dr. Bailor are well trained and experienced in the excisional techniques of skin cancer surgery as well as in the subsequent reconstruction. By planning ahead for the reconstruction, he can plan the most appropriate incision to remove the skin cancer.
Any time that an incision is made in the skin, there will be a scar. The goal is to minimize and camouflage this scar. This is accomplished by orienting the incision to remove the skin cancer in a direction that will leave the least noticeable scar. There are natural lines on the face and neck and when an incision is parallel to one of these lines, the scar is not as evident as one that runs in a different direction. This attention to aesthetics is important to patients, especially when the features of the face are involved.

Excised Skin Cancer

Sutured Incision
Recognizing skin cancer
Basal cell carcinoma and squamous cell carcinoma are the most common types of skin cancer and may appear as:
- A small, white or pink nodule or bump
- Smooth and shiny, waxy or pitted on the surface
- A red spot that’s rough, dry or scaly
- A firm, red lump that may form a crust
- A crusted group of modules
- A sore that bleeds or doesn’t heal after two to four weeks
- A white patch that looks like scar tissue.
Both types enlarge locally and slowly over time and usually do not spread (metastasize) to distant parts of the body. With time, however, either type can invade adjacent structures. Early detection and treatment is key to minimizing the cosmetic defect.
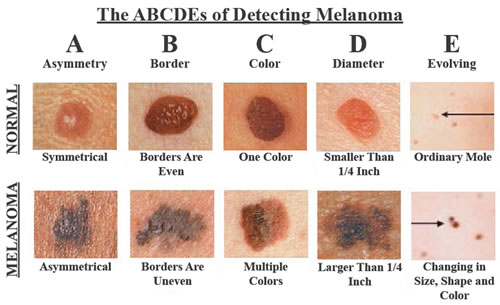
Malignant melanoma is a very aggressive form of skin cancer that can rapidly spread to other vital organs of the body. Accounting for 80% of all skin cancer deaths, malignant melanoma is the deadliest type of skin cancer. It is usually signaled by a change in the size, shape, or color of an existing mole, or as a new growth greater than 6mm in diameter on normal skin.
The ABCDE criteria developed by the American Cancer Society provides an easily remembered guideline to use in self-examination for malignant melanoma.
Other characteristics that alert Dr. Lieberman are ulceration, bleeding or any change in sensation, such as itching. Any lesion that has a history of change warrants a biopsy to make a definitive diagnosis.